By Iris Farrou
22 Apr, 2023
Diet & Exercise, Lifestyle Tips, Menopause, Peri-Menopause, Peri-Menopause, Pregnancy, Prevention, Queer Health, Reproductive health, Sexual health, Women's Health
bladder control, Body Changes In Menopause, bowel function, Childbirth, core strengthening, Early menopause, ease the birthing process, estrogen loss, Frequent urination, Kegel, natural delivery, Pelvic Floor, pelvic floor dysfunction, pilates, Strengthen pelvic floor muscles, stress urinary incontinence, SUI, UTI, vaginal delivery, weak bladder

Maybe the first word that comes to mind when you hear about Pelvic Floor Exercises is “Kegel”! Yes, that’s correct– Kegel exercises are one way to exercise your pelvic floor muscles, but they are not the only ones. Kegel balls have lately become popular as an easier and faster way to strengthen your pelvic floor muscles, increase sexual pleasure, and prevent incontinence (especially if you were Assigned Female at Birth–AFAB). However, there is much debate over them, so before we worry about that we will provide some information on the benefits of pelvic floor exercises in general.
What are the benefits for AFAB people?
- Pelvic floor exercises improve bladder and bowel function control, which can be extremely helpful after childbirth or in older years. It can help with constipation, and with incontinence.
- Strong muscles on your pelvic floor can also significantly reduce the risk of prolapse.
- If you are considering childbirth, they do support vaginal delivery, and strong pelvic muscles will also greatly improve your recovery from childbirth and other gynecological surgeries.
- They are reported to help with vaginal contractions and blood flow during sex, thus increasing sexual satisfaction and orgasmic potential.
Like any self-care routine, and especially an exercise routine that helps you strengthen your muscles, training your pelvic floor muscles can help you increase your social confidence and overall quality of life.
How do they help with pregnancy and delivery?
Your pelvic floor muscles are first in line to be affected if you become pregnant; the weight of your growing baby will undeniably put extra strain on the pelvic floor. In addition to the weight, hormonal changes in pregnancy cause your muscles to soften and stretch more easily. That can lead to bladder/ bowel problems while you are pregnant and after giving birth.
It is recommended to start strengthening your pelvic floor as soon as you learn that you are pregnant. Strong muscles in the area will reduce the risk of bowel or bladder problems during your pregnancy, you will learn how to control your muscles to assist with contractions during childbirth (in the case of vaginal delivery), and with a strong pelvic floor you will return to normal much easier after delivery.
What happens to the pelvic floor after menopause?
After menopause, the production of estrogen in our bodies significantly reduces. This can lead to weaker or stiffer muscles on the pelvic floor. Connective tissues may provide less support, and along with a lifetime of bad habits and lack of specific exercise, we may be in danger of experiencing pelvic floor dysfunction.
The pelvic floor muscles are part of your spine and pelvis. If they are struggling, you may experience pain in your lower back. Weak pelvic muscles can also lead to Stress Urinary Incontinence (SUI), which means you may not be able to control your bladder during seemingly simple activities, like laughing, coughing, or sneezing. More serious pelvic dysfunctions can be pelvic organ prolapse–which can be avoided with pelvic floor rehabilitation–and bowel and urinary urgency, where we may not be able to control the urge to urinate or defecate and incidents of leakage may occur.
No matter your age, it is never too soon or too late to start looking into pelvic floor exercises or rehabilitation that are best for you, your physical condition, and your abilities.
https://www.pelvicfloorfirst.org.au/pages/pelvic-floor-muscle-exercises-for-women.html
https://www.pregnancybirthbaby.org.au/pelvic-floor-exercises
https://provenancerehab.com/aging-and-the-pelvic-floor/
More
By Iris Farrou
14 Apr, 2023
Health Conditions and Pregnancy, Pregnancy, Procedures, Queer Health, Reproductive health, Surrogate, Women's Health
Buffalo NY, Cryogenic, Egg Freezing, Embryo Banking, Embryo Freezing, Fertility, Fertility Assistance, Fertility Preservation, Freezing My Eggs, How to save my eggs, Infertility treatment Buffalo, Oocyte Cryopreservation, Pregnancy and Infertility
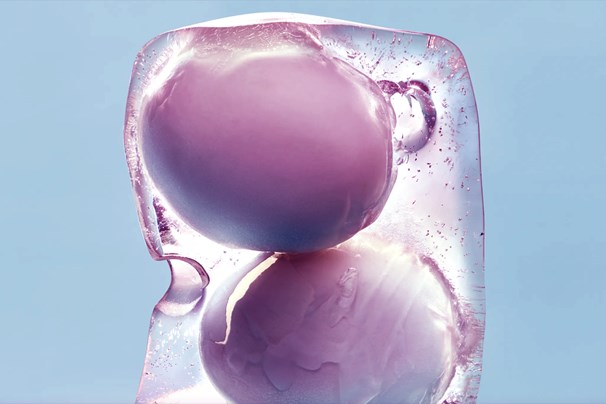
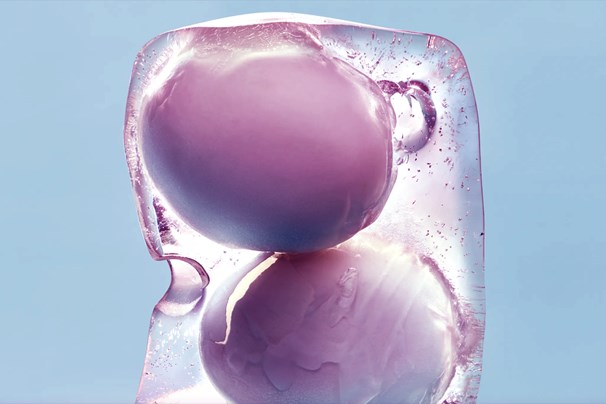
Many people consider the choice of freezing their eggs so they can retrieve them at a later time and start a family. This process is, nowadays, more common than it used to be; there is more information available for people to become aware of the pros and cons, there are more facilities that can store your eggs at an affordable price, and more professionals will suggest it if you want to have your own family later in life, or are undergoing treatments that may affect your fertility.
When Should I Consider it?
Most cis-women reach the peak of their fertility at age 30. While eggs continue to be produced and can be retrieved after that age, our egg production drops significantly around age 37, and completely stops when entering menopause–usually between 45-55 years of age. Patients who are experiencing severe health concerns that may affect their fertility– such as undergoing chemotherapy, having Polycystic Ovarian Syndrome, or endometriosis– may want to consider undergoing fertility treatments and retrieve their eggs for freezing. Egg freezing is also common among individuals who are undergoing hormone replacement therapy.
What is the Process?
It is quite a straightforward process to freeze your eggs, so don’t be alarmed by the terminologies used or the clinical equipment needed. In fact, it is very similar to the process of in-vitro fertilization, with the difference being that the eggs are not fertilized immediately, but frozen. Most cycles are complete in about 2-3 weeks.
- The first step would be to meet with a fertility specialist to discuss your desire to freeze your eggs. Then, you will schedule an exam for complete medical history, bloodwork, and hormone testing. Your doctor may also recommend a transvaginal ultrasound to assess your ovarian reserve.
- You will need to monitor your menstrual cycle and determine the exact dates when you are ovulating. To get more accurate results, your doctor may recommend birth control. After that, you will start stimulating your egg production.
- Most commonly, you will start by injecting 2-3 hormone medications a day for about ten days. This will encourage a group of eggs to develop at the same time.
- To track the ovulation and development of the eggs, you will have frequent blood work done and 4-6 pelvic ultrasounds.
- Once your eggs have matured, they will be retrieved. This involves an ultrasound-guided surgical procedure that takes 20-30 minutes under anesthesia.
And you will have reached the final step! Once an embryologist confirms the eggs are mature, which means they will have the potential to be fertilized, your eggs will head to their deep freeze home: liquid nitrogen tanks in an embryology lab.
https://www.hopkinsmedicine.org/health/wellness-and-prevention/freezing-eggs-preserving-fertility-for-the-future
https://www.healthline.com/health/egg-freezing-process#timeline
More
By Iris Farrou
27 Mar, 2023
Lifestyle Tips, Menopause, Peri-Menopause, Peri-Menopause, Prevention, Queer Health, Reproductive health, Sexual health, Women's Health
Acute UTI, Aging and Painful Sex, Aging and UTIs, Am I going through menopause, Bladder Incontinence, Body Changes In Menopause, Easing the Symptoms of Menopause, Menopause, Pelvic Floor, Prevent urinary tract infection, Urinary Tract Infection, UTI

If you have a vagina, then you have possibly been warned about the dangers of Urinary Tract Infections (UTIs), and the ever-present danger that they may return and not leave you alone. Many women also report they get UTIs so often that they get used to the symptoms– so much so that they don’t realize they have an infection until it gets too bad. Because nobody likes more pain, or more health risks, let’s take a look at the three areas of the urinary tract that a UTI may affect, and the possible symptoms:
| Area |
Symptoms |
| Kidneys |
Nausea, vomiting, back/side pain, shaking and chills, high fever |
| Bladder |
Frequent and painful urination, blood in urine, pelvic pressure, lower belly discomfort |
| Urethra |
Unusual discharge, burning sensation during urination |
Did you know that UTIs are the most common bacterial infection in women over 65? Though young people certainly can suffer from a UTI, untreated UTIs in older women can lead to much more serious health issues, like kidney failure or sepsis. One reason for older women’s susceptibility to UTIs is the weakened muscles in the bladder and pelvic floor, causing incontinence or urinary retention. The longer the urine remains in the urinary tract, the higher the risk of bacterial multiplication.
Another reason why older women are at a higher risk for a UTI is because estrogen levels drop significantly after menopause. This can lead to an imbalance of good and bad bacteria in the vagina, heightening the risk of an infection. It is suggested that post menopausal women use vaginal estrogen creams, which can help support the presence of good bacteria. Drinking plenty of water and fluids, especially cranberry juice, can also help prevent infections.
No matter your age, to lessen the risk of a UTI you should also make sure you are wearing loose clothing, emptying your bladder often, wiping front to back, and always keep an eye out for possible symptoms if you have reason to be concerned. UTIs are usually treated with narrow-spectrum antibiotics, as those are more likely to be accepted by the body. In more advanced cases, UTI patients are hospitalized and receive IV antibiotics.
If you or a loved one use pads or adult diapers, you should make sure to change them often and clean the area well, pat dry, between uses. UTIs can be especially problematic for patients suffering from Alzheimer’s or dementia, as they often cannot communicate their needs or state their symptoms. In those cases, the UTI may escalate to the point where the affected person starts acting erratically, more confused than usual, and even more disoriented. If those symptoms worsen, it is definitely advisable to have elderly female patients be treated by a doctor immediately.
https://www.bannerhealth.com/healthcareblog/better-me/the-risk-of-utis-as-you-age
https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447
More
By Iris Farrou
10 Mar, 2023
Fatherhood, Lifestyle Tips, New Moms, Parenting, Queer Health, Reproductive health, Your baby's health
Baby Etiquette, health tips before meeting newborn baby, Meeting Your Baby, New Parents, Newborn, Visiting a baby, When can I meet a new baby

Whether you are a parent, a close friend, or a family member, the arrival of a newborn is exciting, and no doubt you are looking forward to meeting the new member of the group! Many close family members tend to directly assume they can visit the newborn, while friends and extended family may be a little more careful. However, there is no one-rule-fits-all when it comes to these situations. In fact, the key rule is to check in with the parents first as this is solely their decision: childbirth is a painful and difficult journey, no matter how rewarding it may be. The new family may or may not feel comfortable accepting guests.
What can both guests and hosts do to make this experience enjoyable, and most importantly, safe for the baby?
The 4 DOs
- Discuss with your partner beforehand how you want to handle guests: who is allowed to visit fresh out of the hospital and for how long? Communicate your decisions to family and friends.
- Check in with the new parents about the visit: schedule a visit, check in at the last minute, respect any changes; follow the new family’s rules.
- Be up to date with your vaccines, visit only if you are feeling well, wash your hands before touching the baby, and remove any jewelry from your hands.
- It’s very important to offer to help if you are visiting a family with a newborn: whether that’s bringing a meal, or taking their dog out for a walk, it can be of tremendous help to the new parents.
Here are some actions that are ill-advised when visiting a newborn:
The 4 DON’Ts
- Babies are susceptible to germs and viruses: don’t take your newborn into crowded, or loud, places before they’ve had time to build their immune system. If you need to get out of the house, ask for help taking care of the baby.
- Don’t bring little kids– while no doubt they are also looking forward to meeting the new baby, little kids carry the additional risk of germ exposure. Also, extra visitors can cause more anxiety for the new parents.
- Avoid putting your face close to the baby’s. Adorable as it may be, such close contact is a risk as mouths carry a lot of germs. Don’t be surprised if the parents ask you to wear a mask.
- Don’t take pictures of the baby without the parents’ permission! Most importantly, don’t post pictures on social media without asking the parents first.
Of course, this is not a comprehensive list of what you should or shouldn’t do when visiting a family with a newborn–just some basic rules you should follow to make it more comfortable for the new parents and to avoid any misunderstandings. Some families are ok with much more socialization than you may expect, and may actively seek it, while some others may choose to be more reclusive when they bring their new baby back home from the hospital. Always follow the family’s rules and decisions!
https://www.hopkinsallchildrens.org/ACH-News/General-News/New-Parents-and-Newborns-Are-Visitors-OK
https://www.owletcare.com/blog/7-key-rules-visiting-newborn
More
By Iris Farrou
28 Feb, 2023
Lifestyle Tips, PMS, Prevention, Procedures, Queer Health, Reproductive health, Sexual health, Women's Health
cysts, Fibroid Cluster, Heavy Periods, Infertility help, MRI, Ovarian, Reproductive system disorders, Symptoms, Ultrasound, Uterine Cancer, Uterine Fibroids, Womens Reproductive Health

If you have a uterus, then you already know there are countless issues to keep in mind and a full maintenance schedule for your uterine health. There is yet another concept to add to your list: uterine fibroids. Ideally, your OBGYN or primary care doctor has already talked to you about these. But if this is the first time you come across this term, fear not–uterine fibroids are extremely common, and 99% of the time they are also harmless. However, that does not mean you should ignore them, or that they don’t contribute their fair share of challenges in your cycle.
What are uterine fibroids and how do I know I have them?
Uterine fibroids, also known as leiomyomas, are quite simple: they are noncancerous growths (or tumors, though that word is admittedly scary) made up of the connective tissue and muscle from the wall of the uterus. They can grow solo, or in a cluster, and are most commonly less than 8 inches in diameter– though they can grow larger. Many people with a uterus do not even realize they have uterine fibroids, unless some of the symptoms start becoming more prominent, or you specifically ask your OBGYN to look for them.
The most common signs of uterine fibroids include heavy menstrual bleeding, periods lasting more than a week, bleeding between your periods, frequent urination or difficulty emptying your bladder–usually resulting in a feeling of heaviness in your lower abdomen–constipation, lower back pain, and even pain during sex. These symptoms are definitely not an exclusive list, and presence of such symptoms does not guarantee the only issue is uterine fibroids: if you have concerns, it is advised that you consult with your doctor so you can know exactly what you are dealing with.
How are they diagnosed and treated?
If you are concerned about the presence of uterine fibroids, you can ask to have an ultrasound done to determine the presence of uterine fibroids. The ultrasound can be transabdominal, and/or be done inside your vagina to get pictures of the uterus. Your doctor may also order blood count tests to determine if you have anemia from chronic blood loss, and to rule out other bleeding disorders. If these methods do not yield satisfactory results, there are more in depth tests that your OBGYN can order, such as an MRI, hysterosonography, or hysteroscopy.
Since uterine fibroids are benign, the recommended treatment–as long as they are not causing significant issues in your day to day life and do not interfere with your fertility–is to keep an eye on them. They rarely grow and do not tend to interfere with fertility and/or pregnancy, and also tend to shrink after menopause. There are possible medications that your doctor may prescribe, medication which control your hormone levels to create menopause-like conditions. This tricks the fibroids into thinking your body has entered menopause, and causes them to shrink along with their unpleasant effects (such as heavy bleeding). Though there are procedures available as well, this is a step you would discuss at length with your doctor.
https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294
https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids#diagnosis-and-tests
More
By Iris Farrou
23 Feb, 2023
Geriatric Mental Health, Heart health, Lifestyle Tips, Mental Health, Nutrition, Queer Health, Women's Health
aging parents, Buffalo OBGYN, Caring For My Elderly Parents, Changes with Aging, Elderly Parents, Family Dynamics, Geriatric, Grandparent Mental Health, Helping Parents with Disabilities, Multi-generation Families, OBGYN, Retired Parents

With the rising costs of living, it is becoming more and more common for families to be multi-generational and house family members of all ages under one roof. More often than not, this means that elders move in with their adult children, who may have their own young families. This is an option that families decide on between themselves, for a variety of reasons, and sometimes it is more financially feasible than living in an elders’ community or a home. In addition to the psychological and communication factors that come into play with such a decision, there are also practical accommodations that need to be considered– which are often overlooked when the aging family member appears able-bodied, but can cause serious trouble if not addressed.
Psychological and Communication Factors
If a new family member joins your existing family, this will necessarily change the family dynamic. All members of the welcoming family need to discuss the options available to them and decide whether adding an aging parent to their household is something they are comfortable doing. Of course, aging parents need to have a say in this: many people are not comfortable with the idea of being a dependant, or with the need to adjust to someone else’s schedule. It is a difficult transition for both parties, and it needs to be treated carefully. Keep in mind that in addition to the behavioral adjustments and changes, there will also be a need for practical changes in the home itself.
Practical Changes
There is a reason why many restaurants and facilities ensure they are ADA compliant, and similar adjustments need to be made in a home where an elderly person resides. The simplest examples of this would be to ensure there is a step-free entry, ideally one that can accommodate a wheelchair and/or walker. Of course, that also means there is a bedroom and full bathroom on the ground floor–possibly enforced with safety amendments like a handrail, non-slip mats, a shower chair, and raised toilet seat.
Practical adjustments don’t necessarily mean that your house will end up looking like a hospital–this popularized, and terrifying, idea only comes around when we talk about in-home hospice, for serious cases. However, basic adjustments do mean that your home will look different, and will probably not have any throw rugs: they are the number one tripping hazard for elderly people, along with pets who are not contained.
Diet and Healthcare
Another common change usually involves keeping tabs on the elderly person’s healthcare, and making adjustments to the usual diet to accommodate their needs. This can range from keeping track of medications, and securing them so that only the person who needs them has access to them, to scheduling doctor appointments, ensuring transportation, interpreting medical results, and advocating for the person you are caring for.
https://www.fda.gov/consumers/womens-health-topics/caring-others-resources-help-you
https://www.aarp.org/caregiving/home-care/info-2018/living-with-aging-parents.html?intcmp=AE-CAR-CAH-EOA1
More
By Iris Farrou
15 Feb, 2023
Fatherhood, Parenting, Pregnancy, Queer Health, Reproductive health, Women's Health
Birth Plan, Emergency Pregnancy Plan, Giving Birth, Giving Birth Checklist, Labor, Planning Birth, Planning for Birth, Planning for Labor, Preparing for Labor
 If you are an expectant mother, and relatively close to delivery, you may have already started working on your birth plan. Or, you may be gathering information and becoming informed even while you are planning your pregnancy! Regardless of your timeline, it’s always a good time to consider your birth plan. Perhaps you have already heard that no delivery will go according to plan, and you need to have different options. While this is true, the suggested rule of thumb is to be well informed and flexible, as you may have to make last minute decisions and consider emergency changes; the goal is for the baby and the delivering mother to be safe and healthy.
If you are an expectant mother, and relatively close to delivery, you may have already started working on your birth plan. Or, you may be gathering information and becoming informed even while you are planning your pregnancy! Regardless of your timeline, it’s always a good time to consider your birth plan. Perhaps you have already heard that no delivery will go according to plan, and you need to have different options. While this is true, the suggested rule of thumb is to be well informed and flexible, as you may have to make last minute decisions and consider emergency changes; the goal is for the baby and the delivering mother to be safe and healthy.
There are sample birth plans available in a variety of websites, but no plan is as good as the one you create yourself, personalize with your own tone and preferences, and one that addresses your medical team directly. Consider your birth plan a direct request to your OBGYN and the nurses that meet you at the labor and delivery ward. It should be easy to read, 1-2 pages long, formatted with bullet-points, personal statements and politely phrased requests; this shows you are well informed, educated, and engaged in your delivery process and take a serious interest in the delivery of your baby. If your birth plan decisions are based on medical conditions or previous delivery experiences, don’t hesitate to include a short description of those as well– it helps your medical team to know why your wishes are there.
Check-off lists and pre-written birth plans almost never address the most important decisions during delivery: pain management and c-sections. In an ideal world, you would have completed a child-preparation program before creating your birth plan. While this may not always be possible, you can consider a book or video course. However, what will really help is for you to tour your birthing facility and learn of the options offered for birthing position, pain management, and newborn care. This is abundantly helpful especially if you require specific props for your birthing positions. If, for example, you request a birthing stool or bar, you need to ensure not only that your birthing facility has those available for you, but also that you are personally educated on how to use them.
Keep in mind that you need to have a contingency plan in place, in case your initial wishes need to be adapted for your safety and the health of your baby. Though very few women opt for a C-section, you always need to be prepared for one. Note in your plan if you wish to receive medications that affect your consciousness, if you want to receive Pitocin for labor augmentation, and whether or not you want to receive an epidural. In case you decline an epidural, you should explain in your birth plan how you have prepared for this decision and what your pain-management plan is.
The scary parts of your birth plan are the most important, almost like two sides of the same coin. Remember that you can, and should, write personal choices and wishes in your birth plan as well: who do you want present during labor, if you wish to place limitations on visitors, any allergies you may have, the contact information of your delivery team (partner, family or friends, doula, OBGYN, etc.), your wishes for newborn care and immediate postpartum care and preferences. Personalize your birth plan and go over it with your doctor, and those responsible for caring and supporting you, well in advance of your due date.
https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/birth-plan/
https://childrensmd.org/uncategorized/writing-a-birth-plan-10-essential-tips-from-a-pediatrician-and-mom-of-5/
More
By Iris Farrou
07 Feb, 2023
Health Conditions and Pregnancy, Lifestyle Tips, New Moms, Nutrition, Pregnancy, Queer Health, Women's Health
Healthy weight gain pregancy, How much weight should I gain in pregnancy, How to manage weight during pregnancy, Normal weight gain during pregnancy, Pregnancy diet, Pregnancy Nutrition
 If you are expecting, or are thinking of becoming pregnant, it is possible that you are also worried about your body weight. Many expecting mothers have faced this worry before, as pregnancy significantly alters your body and is expected (and should) increase your body weight. At the same time, you want to make sure that you experience a healthy pregnancy and don’t put yourself or your baby in danger. First of all, you should remember your baby weighs around 7-8 pounds– that’s a big chunk of pregnancy weight! Additionally, your placenta, a larger uterus, and amniotic fluid add about 2 pounds each. You will also experience an increased blood volume of 3-4 pounds, and increased fluid volume of 2-3 pounds, as well as larger breasts which add 1-3 pounds. It is important to remember that your fat stores, which are much needed for a healthy pregnancy and delivery, will add 6-8 pounds.
If you are expecting, or are thinking of becoming pregnant, it is possible that you are also worried about your body weight. Many expecting mothers have faced this worry before, as pregnancy significantly alters your body and is expected (and should) increase your body weight. At the same time, you want to make sure that you experience a healthy pregnancy and don’t put yourself or your baby in danger. First of all, you should remember your baby weighs around 7-8 pounds– that’s a big chunk of pregnancy weight! Additionally, your placenta, a larger uterus, and amniotic fluid add about 2 pounds each. You will also experience an increased blood volume of 3-4 pounds, and increased fluid volume of 2-3 pounds, as well as larger breasts which add 1-3 pounds. It is important to remember that your fat stores, which are much needed for a healthy pregnancy and delivery, will add 6-8 pounds.
Though these amounts may differ from person to person, the general weight added to a mother’s body by the end of pregnancy is about 30 pounds. Most expectant mothers gain 1-5 pounds in the first trimester and 1-2 pounds per week in the second and third trimester. According to the American Pregnancy Association, a pregnant woman of relatively normal weight who gets less than half an hour of exercise every week should have a calorie intake of 1,800 in the first trimester, 2,200 in the second trimester, and 2,400 in the third trimester. It is suggested that you limit processed foods, sugars, and extra fats when you are thinking about your diet while pregnant.
The first idea that pops into mind when thinking about a healthy diet during pregnancy is supplements and vitamins. Though these are definitely important, and prenatal vitamins ensure you don’t miss out on key nutrients, you do need to decide on the specifics by consulting with your doctor or healthcare provider. It is ideal to start taking a daily prenatal vitamin at least three months before conception. Discuss your options with your doctor before deciding, as supplements need to be tailored to add on to your current diet, any special diet, health conditions, and you need to know about possible supplements that do not have a good track record and may harm your pregnancy.
Other than supplements, the principle of any healthy diet applies to pregnancy as well– make sure you consume plenty of fruits, vegetables, whole grains, healthy fats, and lean protein. Here are the nutrients that deserve special attention during your pregnancy:
- Folate and Folic Acid: this helps decrease the risk of premature birth or low birth weight. It is also a B vitamin that helps the healthy development of the brain and spinal cord.
- Calcium: you may already know calcium is necessary for healthy bones and teeth, and both you and your baby need it. Did you know that calcium also helps the circulatory, muscular, and nervous systems?
- Vitamin D: this can work together with calcium to ensure healthy bones and teeth. Vitamin D is most commonly found in fatty fish, fortified milk, and orange juice.
- Protein: you want to keep on intaking protein throughout your pregnancy as it supports your baby’s overall growth and development. You need at least 71 grams a day.
- Iron: remember that during pregnancy you need double the amount of iron that non-pregnant persons need. The body uses iron to make hemoglobin, a protein in the red blood cells that carries oxygen to the body’s tissues. If you don’t get enough iron during your pregnancy, you may be at risk of developing anemia.
https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/pregnancy-weight-gain/
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-nutrition/art-20045082
More
By Iris Farrou
13 Jan, 2023
Menstruation, Prevention, Queer Health, Reproductive health, Sexual health, Women's Health
Abnormal Discharge, Ph Balance, vaginal discharge, Vaginal Odors, When to See a Gynecologist, yeast infection

Let’s get one thing out of the way: all vaginas produce some odor, and this odor varies through your menstrual cycle and through life’s activities. For example, you are more likely to experience a stronger smelling vaginal discharge if you are mid-cycle, after intercourse, or after a workout. However, if there is an unfamiliar, strong, and unpleasant odor that persists for several days that is cause for concern and should be checked out ASAP. If it is accompanied by other symptoms like grayish vaginal discharge, itching and burning, then it may be a sign of a health issue as well.
The most common reason for a concerning vaginal odor is an imbalance in your vaginal pH; if your vaginal flora is imbalanced that may produce an unfamiliar smell. Some of those odors can be short term, and not a cause for concern. For example, if you are menstruating you may notice a coppery smell–that’s because period blood contains iron. A slight ammonia odor may be a sign that you are dehydrated or there is urine residue on your genitals. A smell similar to body odor can be a sign that you are stressed and your sweat glands are working overtime.
Temporary changes in your vaginal odor are normal, and they are not always a cause for concern. If bad odor persists, however, you may want to look into one or more of the following possible causes: bacterial vaginosis, which is an infection caused by an imbalance in your vaginal pH; trichomoniasis–a sexually transmitted infection caused by a parasite; changes in your vaginal odor due to pregnancy; postpartum vaginal odor. Some rare causes for vaginal odor can also be rectovaginal fistula–an extremely rare condition where the opening between our rectum and vagina allows feces to leak into your vagina; vaginal cancer or cervical cancer.
Treatments
Before you jump into panic mode, and especially if you have just noticed an unpleasant odor down there, you can try the following simple methods to eliminate symptoms (considering they are non threatening):
- Sometimes we just need a really good shower, or more regular showers: if you are working out more, have intercourse more often, or are even way more stressed than usual, that may change your odor.
- Do not wash inside your vagina: you definitely want to use appropriate products to wash the outside areas of your vagina, but do not use water, soap, or a washcloth inside your body.
- Check for product changes: did you recently change your vaginal wash? You may have a sensitivity to a new ingredient, or a new detergent. Even underwear fabrics and tight clothes can cause irritation and a different smell.
- Stay hydrated and eat a balanced diet: strong foods like onion, garlic, asparagus and oily fast foods can cause your body to produce not-so-pleasant odors.
https://my.clevelandclinic.org/health/symptoms/17905-vaginal-odor
More
By Iris Farrou
08 Dec, 2022
Fatherhood, Heart health, Lifestyle Tips, Mental Health, New Moms, Parenting, Postpartum, Pregnancy, Procedures, Queer Health, Reproductive health, Surrogate, WNY Ob-Gyn News, Women's Health, Your baby's health

You have probably heard of couples using surrogate mothers to conceive, or carry a pregnancy to term. The term is often associated with a couple’s fertility challenges, and difficult as those may be, it doesn’t stop being a wonderful way for a couple to have a baby– the parents who initiate the process are called the “intended parents,” and the individual carrying the fetus is the “surrogate mother.” Some of the reasons parents-to-be consider surrogacy may be:
- Trouble conceiving through IVF, which may be related to infertility of unknown origin
- Medical issues that affect the uterus, or even a previous hysterectomy
- Conditions that make the pregnancy too high-risk, such as health concerns or advanced maternal age
- Queer couples
If you didn’t know it, there are two types of surrogacy: traditional one and gestational surrogacy.
Traditional Surrogacy: this is the least commonly used method of surrogacy as it comes with more legal and emotional complexities. In traditional surrogacy, the surrogate is both the egg donor and the surrogate mother. She uses her own eggs, and therefore has a genetic relationship to the baby. During this method, the surrogate is impregnated using intrauterine insemination. The doctor uses sperm provided by the intended father, transfers it into the uterus of the surrogate, and natural fertilization of the egg takes place from then on. As medical science advances, this type of surrogacy becomes increasingly less common.
Gestational Surrogacy: this is the most commonly used type of surrogacy, and there is no genetic relationship between the surrogate mother and the fetus. Instead, an embryo is inserted into the surrogate’s uterus and she carries the pregnancy to term for the intended parents. To get to that point, the intended parents provide sperm and eggs–or use either/or from a donor–fertilize them and then have them inserted into the surrogate mother’s uterus using in vitro fertilization. In this type of surrogacy, the surrogate may be also called gestational carrier.
Why this choice?
As mentioned above, there are several health reasons why intended parents may choose to find a surrogate mother. However, the decision does not have to rely on those health reasons, and it is always deeply personal and a private decision. The most common reason people choose surrogacy over adoption is that they want to have a biological connection to their child; even though familial bonds are not necessary to build a strong, happy, and healthy family, many parents do want a biological connection to their offspring.
Surrogacy offers a safe and transparent pregnancy as the intended parents are there every step of the way. The most common concern with adoption is that the future parents do not know the medical history of the birth mother, or the father. This can raise serious concerns about their future baby’s medical history, and many parents feel uneasy not knowing whether their adoptive infant may have potentially been exposed to malnourishment or toxins in-utero.
If you are considering a surrogate option for your family, consult with your family doctor first, and keep in mind you may also need to review your state’s laws around surrogacy agreements.
https://www.surrogateparenting.com/blog/what-is-a-surrogate-mother/
https://www.fertilitypreservation.org/blog/when-to-consider-surrogacy-and-how-to-choose-the-right-one
More